Thank you for visiting The Second9Months in Seattle, Washington!
I accept **AETNA and **UNITED insurance. Many insurance companies offer full reimbursement.
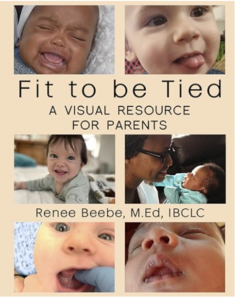
New resource available for parents and the professionals who support them! Check out my new book on Amazon
**Information Regarding This Practice and Corona Virus**
We understand that you may have concerns about contact with people outside your family right now, but that doesn’t change the fact that you may need help! We are happy to address your concerns.
You have 2 choices for a comprehensive consultation:
Virtual consultations. Virtual consultations can be surprisingly effective with an experienced provider. We use a HIPAA compliant, secure platform to ensure your privacy. It’s easy to request an appointment! (Aetna subscribers: Aetna no longer pays IBCLCs for telehealth). A super bill will be provided to clients with other insurance and many insurance plans do reimburse a portion or all of the fee. For more information about virtual consultations, please see this post.
Home visits: I am doing home visits on a limited basis, since most families like the convenience of virtual. For home visits I have extra precautions in place to keep everyone safe and you will need to consent to my Covid Policies prior to the visit. I can bill Aetna and United directly for home visits. For other insurance a superbill is provided.
If you need help with breastfeeding, call now! (206) 356-7252. (no texts please) or request an appointment here. I answer calls and emails promptly. (Phone is fastest!) Breastfeeding support is available 7 days a week: Home or office visits, phone or virtual consultations. You decide.

Not in Seattle? No problem! I do video conferencing all over the world! Request an appointment!
If there was a <3 (heart) button for the amount of help you provided to my family, I would totally click it! LB
General support for moms in Seattle area–No appt. necessary. For a virtual breastfeeding support group, please request to join my local (Seattle area) facebook support group:
Breastfeeding and Pumping Support in Seattle.
I wish you had been at the hospital with us when our baby was first brought to us for breastfeeding. Your manner was very patient, incredibly understanding, superbly attentive, and extremely calm. You shared an incredible depth of knowledge. Thank you!
Experience Counts! Seattle area mothers choose me because of my vast experience and my reputation in the community. Over 25 years helping breastfeeding adds up to over 4000 babies!
My pediatrician called you ‘one of the best lactation consultants in the region.’ Wow!
Other Stuff:
Check out my new products platform for free PDFs and classes for parents!
Sign up for my informative quarterly newsletter.
Thanks very much for all these newsletters to keep in touch! I can never forget your great help to overcome the challenges I had with breastfeeding both of my babies.
Help someone else receive lactation help. Donate to the Lactation Fund. Any amount will help low income parents with breastfeeding challenges.
If you’d like more information on how I can help you, visit the services page, Frequently Asked Questions, or simply give me a call! (206) 356-7252
Renee Beebe second9months@gmail.com


 Having low milk supply can be very difficult for people –especially when they’ve always wanted to breastfeed. People will do almost anything to increase supply. They research formula, learn about things like “refill rate,” supplementation methods and herbs and foods for milk supply. This mom had an aha moment which helped her look at her situation with a different lens. She is shown here nursing her baby with a homemade supplementer. Thank you so much for generously sharing your thoughts with all of us!
Having low milk supply can be very difficult for people –especially when they’ve always wanted to breastfeed. People will do almost anything to increase supply. They research formula, learn about things like “refill rate,” supplementation methods and herbs and foods for milk supply. This mom had an aha moment which helped her look at her situation with a different lens. She is shown here nursing her baby with a homemade supplementer. Thank you so much for generously sharing your thoughts with all of us!